Skin rashes are among the most common dermatological conditions affecting people of all ages. These inflammatory reactions of the skin can range from mild, temporary irritations to signs of serious underlying health issues. Understanding how to identify different types of rashes can help determine appropriate treatment approaches and when medical intervention is necessary.
With countless potential causes—from allergies and infections to genetic factors and environmental irritants—skin rashes present in remarkably diverse ways. This comprehensive guide explores 15 common skin rashes, providing detailed information on their distinctive characteristics, causes, and management strategies.
Skin rashes affect millions worldwide, with some studies suggesting up to 31% of adults experience some form of dermatitis during their lifetime. These inflammatory skin conditions manifest through various symptoms, including redness, itching, scaling, bumps, blisters, or changes in skin texture and appearance.
Proper identification of skin rashes is crucial for effective treatment. Misdiagnosis can lead to inappropriate interventions that may worsen symptoms or delay necessary care. While many rashes resolve with simple home remedies, others require medical attention to prevent complications or address underlying health concerns.
Generally, you should seek medical care for rashes that:
- Cover a large portion of your body
- Appear suddenly and spread rapidly
- Are accompanied by fever, pain, or signs of infection
- Develop blisters or open sores
- Don’t improve with over-the-counter treatments
- Interfere with daily activities or sleep
Contact Dermatitis
Contact dermatitis occurs when your skin reacts to something it touches, resulting in a localized inflammatory response. This condition affects approximately 20% of people at some point in their lives.

Identifying Symptoms
Contact dermatitis typically presents as:
- Redness and inflammation confined to the area of contact
- Intense itching or burning sensation
- Skin swelling and tenderness
- Formation of small, fluid-filled blisters that may weep or crust
- Dry, cracked, or scaly skin in chronic cases
Common Triggers
Contact dermatitis falls into two primary categories:
Irritant contact dermatitis (accounting for 80% of cases) results from substances that directly damage the skin, including:
- Soaps, detergents, and cleaning products
- Industrial chemicals and solvents
- Acids and alkalis
- Prolonged water exposure
Allergic contact dermatitis occurs when the immune system reacts to specific allergens:
- Nickel and other metals in jewelry
- Plants like poison ivy, oak, and sumac
- Preservatives and fragrances in cosmetics
- Latex, adhesives, and rubber compounds
- Topical medications (neomycin, bacitracin)
Home Care and Prevention
Managing contact dermatitis begins with identifying and avoiding the offending substance. Additional strategies include:
- Washing the affected area with mild soap and cool water to remove irritants
- Applying cool, wet compresses to reduce inflammation and itching
- Using over-the-counter hydrocortisone cream (1%) for temporary relief
- Taking oral antihistamines to reduce itching and help with sleep
- Moisturizing regularly with fragrance-free products
- Wearing protective clothing or gloves when handling potential irritants
Atopic Dermatitis (Eczema)
Atopic dermatitis, commonly known as eczema, is a chronic inflammatory skin condition affecting up to 20% of children and 3% of adults worldwide. This condition typically runs in families and is often associated with other atopic conditions like asthma and allergic rhinitis.
Characteristic Appearance
Eczema’s appearance varies by age and can affect different body areas:
- Infants: Rash typically appears on the face, scalp, and extensor surfaces of arms and legs
- Children: Rash often affects flexural areas (inside of elbows, behind knees)
- Adults: May develop on hands, eyelids, and flexural areas
Distinctive features include:
- Intense itching, often worse at night
- Dry, red, and inflamed skin
- Small, fluid-filled bumps that may weep when scratched
- Rough, leathery skin from chronic scratching (lichenification)
- Visible excoriations and potential secondary infections
Causes and Risk Factors
Atopic dermatitis develops through a complex interplay of:
- Genetic factors: Mutations in the filaggrin gene that maintains skin barrier function
- Immune system dysfunction: Hyperactive inflammatory response
- Environmental triggers: Irritants, allergens, stress, climate conditions
- Microbiome imbalance: Increased Staphylococcus aureus colonization
Management Techniques
Effective eczema management requires a multifaceted approach:
- Daily moisturizing: Apply emollients at least twice daily, especially after bathing
- Gentle skin care: Use fragrance-free, hypoallergenic products; take short, lukewarm showers
- Trigger avoidance: Identify and minimize exposure to personal triggers
- Anti-inflammatory treatments: Topical corticosteroids or calcineurin inhibitors for flares
- Infection prevention: Address signs of infection promptly
- Stress management: Practice relaxation techniques and adequate sleep hygiene
Psoriasis
Psoriasis is a chronic immune-mediated condition affecting approximately 2-3% of the global population. This non-contagious disease accelerates skin cell turnover, causing cells to build up rapidly on the skin’s surface.
Visual Identification
Psoriasis has several distinctive forms, with plaque psoriasis being most common (affecting 80-90% of patients). Key visual characteristics include:
- Well-defined, raised red plaques covered with silvery-white scales
- Symmetrical distribution, often on elbows, knees, scalp, and lower back
- Skin that may crack, bleed, or become painful (especially during flares)
- Nail changes including pitting, ridging, or separation from the nail bed
- Inverse psoriasis appears as smooth red patches in skin folds without scaling
Underlying Causes and Triggers
Psoriasis develops from complex interactions between:
- Genetics: Over 60 gene variants linked to psoriasis susceptibility
- Immune dysfunction: Overactive T-cells and inflammatory cytokines
- Environmental triggers:
- Stress and psychological factors
- Skin injuries (Koebner phenomenon)
- Infections, particularly streptococcal throat infections
- Certain medications (beta-blockers, lithium, antimalarials)
- Alcohol consumption and smoking
- Cold, dry weather conditions
Treatment Options
Psoriasis management is tailored to severity, type, and individual factors:
- Topical treatments: Corticosteroids, vitamin D analogs, retinoids, coal tar
- Phototherapy: UVB or PUVA (psoralen plus UVA) treatments
- Systemic medications: Methotrexate, cyclosporine, acitretin for moderate-to-severe cases
- Biologics: Target specific immune pathways (TNF-alpha, IL-17, IL-23 inhibitors)
- Lifestyle modifications:
- Maintaining healthy weight (obesity worsens psoriasis)
- Avoiding trigger foods (individualized)
- Regular exercise and stress management
- Moisturizing routinely with emollient-rich products
- Limiting alcohol consumption
- Smoking cessation
Seborrheic Dermatitis
Seborrheic dermatitis affects approximately 5% of the general population, with higher prevalence in infants (cradle cap) and adults between 30-60 years. This chronic, relapsing condition is associated with the yeast Malassezia and affects sebum-rich areas.
Distinctive Symptoms
Key characteristics of seborrheic dermatitis include:
- Greasy, yellowish or white scales and flakes
- Underlying skin redness and inflammation
- Mild to moderate itching (less intense than other dermatitis types)
- Burning sensation in some cases
- Cyclical pattern with flares and remissions
Commonly Affected Areas
Seborrheic dermatitis specifically targets areas with numerous sebaceous glands:
- Scalp: Ranging from mild dandruff to thick, adherent scales
- Face: Eyebrows, sides of nose, eyelid margins (blepharitis)
- Behind the ears: Often overlooked but commonly affected
- Central chest: May present as small, scaly patches
- Body folds: Intertriginous areas including armpits, groin, under breasts
Home Treatments
Managing seborrheic dermatitis involves both regular maintenance and treating flares:
- Medicated shampoos: Containing active ingredients like:
- Pyrithione zinc (antibacterial and antifungal)
- Selenium sulfide (reduces Malassezia proliferation)
- Ketoconazole (antifungal)
- Salicylic acid (helps remove scales)
- Coal tar (reduces cell turnover and inflammation)
- For facial involvement:
- Gentle cleansing with non-soap cleansers
- Over-the-counter antifungal creams
- Brief use of low-potency hydrocortisone for flares
- Lifestyle adjustments:
- Stress management techniques
- Regular washing of bedding and headwear
- Avoiding harsh skincare products
Heat Rash (Miliaria)
Heat rash, medically known as miliaria, occurs when sweat ducts become blocked and trapped beneath the skin. This condition is common in hot, humid environments and affects people of all ages, though infants are particularly susceptible.
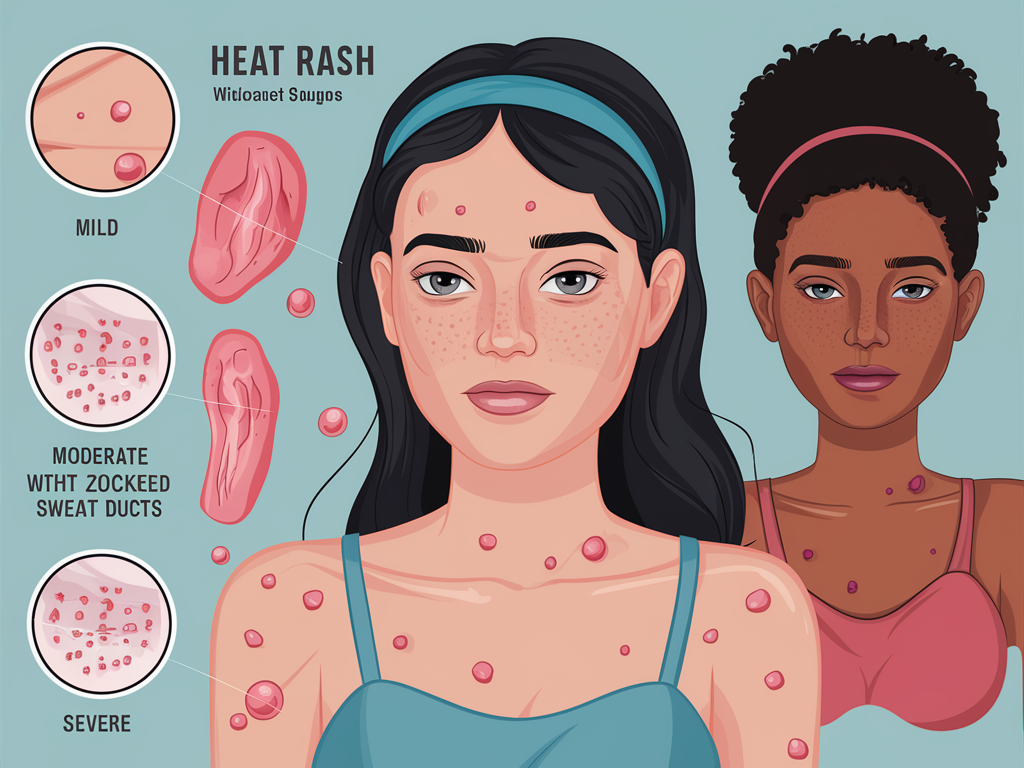
Appearance and Sensation
Heat rash presents in several forms, depending on how deeply sweat is trapped:
- Miliaria crystallina (superficial): Clear, fluid-filled blisters that break easily
- Miliaria rubra (prickly heat): Small, red, itchy bumps with intense prickling sensation
- Miliaria profunda (deep): Flesh-colored, firm bumps that don’t itch but may cause discomfort
- Miliaria pustulosa: When the rash becomes infected, developing pus-filled bumps
Common sensations include:
- Intense itching or prickling
- Burning feeling
- Reduced or absent sweating in affected areas
How Overheating Leads to Blocked Sweat Ducts
Heat rash develops through a cascade of events:
- Excessive sweating occurs due to heat, exercise, fever, or occlusive clothing
- Sweat duct openings become obstructed by:
- Dead skin cells
- Bacterial biofilms
- Prolonged maceration of the skin
- Certain skincare products or medications
- Trapped sweat causes pressure and inflammation in surrounding tissues
- Sweat leaks into adjacent skin layers, causing characteristic symptoms
Cooling Methods and Prevention
Heat rash typically resolves spontaneously when the skin cools, but several approaches can accelerate healing and prevent recurrence:
- Immediate relief:
- Move to cooler, less humid environments
- Apply cool compresses
- Take cool showers or baths
- Use calamine lotion for itching
- Apply cornstarch or talc-free powder to absorb moisture (avoid in infants)
- Prevention strategies:
- Wear loose-fitting, lightweight, breathable fabrics (cotton, linen)
- Use air conditioning or fans during hot weather
- Take breaks from physical activity in hot conditions
- Avoid occlusive ointments and heavy creams in hot weather
- Change wet clothing promptly
- Keep skin clean and exfoliate gently to prevent duct blockage
Hives (Urticaria)
Hives, or urticaria, affects up to 20% of people at some point in their lives. These itchy welts result from the release of histamine and other inflammatory mediators from mast cells in the skin.
Identifying Welts and Wheals
Hives have distinctive characteristics:
- Raised, red or skin-colored welts with clearly defined edges
- Size varying from a few millimeters to several centimeters
- Blanching (whitening) when pressed
- Individual welts typically resolve within 24 hours, though new ones may form
- Can appear anywhere on the body and may change shape or migrate
- Often accompanied by angioedema (swelling of deeper tissue layers, especially around eyes and lips)
Allergic and Non-Allergic Triggers
Hives can be triggered by numerous factors:
- Allergic reactions to:
- Foods (especially shellfish, nuts, eggs, dairy)
- Medications (antibiotics, NSAIDs, opiates)
- Insect stings or bites
- Latex
- Animal dander
- Non-allergic causes:
- Physical stimuli (pressure, cold, heat, sunlight, vibration)
- Exercise
- Emotional stress
- Infections (viral, bacterial, parasitic)
- Autoimmune conditions
- Dermatographism (“skin writing”)
Relief Strategies and Emergency Care
Most acute hives cases resolve within hours to days, but management includes:
- Home treatment:
- Oral antihistamines (H1 blockers like cetirizine, loratadine)
- Cool compresses or cool baths with colloidal oatmeal
- Loose-fitting clothing
- Avoiding hot showers and known triggers
- Stress reduction techniques
- When to seek emergency care:
- Difficulty breathing or swallowing
- Swelling of tongue or throat
- Feeling faint or dizzy
- Nausea or vomiting accompanying hives
- Rapid pulse
- Chronic urticaria treatment:
- Higher-dose antihistamines
- H2 blockers (famotidine, ranitidine)
- Leukotriene modifiers
- Biologics (omalizumab)
- Immunosuppressants if autoimmune in origin
Athlete’s Foot (Tinea Pedis)
Athlete’s foot is a common fungal infection affecting approximately 15-25% of the population. This highly contagious condition is caused primarily by dermatophytes, fungi that feed on keratin in the skin.
Recognizing Symptoms
Athlete’s foot presents in several clinical patterns:
- Interdigital type (most common):
- Scaling, peeling, and cracking between toes (especially 4th and 5th)
- Itching and burning sensation
- Maceration and whitish appearance
- Moccasin type:
- Chronic dry scaling covering the entire sole
- Thickened, cracked skin extending up sides of foot
- Occasional nail involvement (onychomycosis)
- Vesicular type:
- Fluid-filled blisters on instep or sole
- Intense itching
- Potential for secondary bacterial infection
Fungal Infection Causes and Transmission
Athlete’s foot spreads through:
- Direct contact with infected individuals
- Contact with contaminated surfaces (shower floors, pool decks, locker rooms)
- Sharing footwear or towels with infected individuals
Risk factors include:
- Wearing tight, enclosed footwear for prolonged periods
- Excessive sweating (hyperhidrosis)
- Walking barefoot in public areas
- Warm, humid conditions
- Minor skin or nail injuries
- Compromised immune system
Over-the-Counter Treatments and Prevention
Effective management includes:
- Antifungal medications:
- Azoles (clotrimazole, miconazole) – apply 2-3 times daily
- Allylamines (terbinafine) – faster action, can apply once daily
- Undecylenic acid preparations
- Treatment protocols:
- Continue treatment 1-2 weeks after symptoms resolve
- Apply to entire foot, not just affected areas
- Consider oral antifungals for severe or resistant cases (prescription required)
- Prevention habits:
- Thoroughly dry feet after washing, especially between toes
- Wear moisture-wicking socks and change them daily or when damp
- Alternate footwear to allow shoes to dry completely
- Use antifungal powder in shoes
- Wear sandals in public showers and pool areas
- Avoid sharing footwear, towels, or nail tools
Ringworm (Tinea Corporis)
Despite its name, ringworm is not caused by a worm but by fungal species similar to those causing athlete’s foot. This highly contagious infection affects the superficial layers of skin on the body.
Characteristic Ring-Shaped Pattern
Ringworm presents with distinctive features:
- Circular or oval-shaped patches with raised, red borders
- Clearer, scaly centers creating a ring-like appearance
- Potential for multiple rings that may overlap
- Mild to intense itching
- Borders that may be vesicular (small blisters) or pustular
- Lesions that enlarge gradually if untreated
How the Fungal Infection Spreads
Ringworm transmission occurs through:
- Direct contact:
- Skin-to-skin contact with infected individuals
- Contact with infected animals (especially cats, dogs, and farm animals)
- Indirect contact:
- Sharing personal items (clothing, towels, bedding, hairbrushes)
- Contact with contaminated surfaces (gym equipment, mats)
- Handling contaminated soil (rarely)
The fungi can remain viable on surfaces for 12-20 months, making environmental contamination significant.
Antifungal Treatment Options
Effective ringworm management includes:
- Topical antifungals:
- First-line treatment for limited lesions
- Apply to lesions and surrounding 2cm of normal skin
- Options include clotrimazole, miconazole, terbinafine, and ketoconazole
- Continue for 1-2 weeks after visual clearing
- Oral antifungals (prescription required) for:
- Extensive involvement
- Hair-bearing areas (scalp, beard)
- Immunocompromised patients
- Infection resistant to topical treatment
- Hygiene practices:
- Wash bedding and clothing daily in hot water during treatment
- Avoid sharing personal items
- Screen and treat household pets
- Wash hands thoroughly after treating lesions
- Keep affected areas clean and dry
- Avoid scratching to prevent spread and secondary infection
Pityriasis Rosea
Pityriasis rosea is a self-limiting skin eruption that typically affects young adults between ages 10-35. This distinctive rash follows a predictable pattern and course, lasting approximately 6-8 weeks in most cases.
Herald Patch and Christmas Tree Pattern
Pityriasis rosea has a unique presentation sequence:
- Herald patch (initial lesion):
- Single, oval or round patch, 2-10cm in diameter
- Salmon-pink or tan color with a slightly raised border
- Fine scale that may detach at the center, creating a “collarette” appearance
- Typically appears on trunk or proximal extremities
- Precedes widespread eruption by 1-2 weeks
- Secondary eruption:
- Multiple smaller lesions (0.5-1.5cm) resembling the herald patch
- Distribution following skin tension lines in a “Christmas tree” pattern
- Predominant on trunk, particularly the back
- Less common on face, scalp, palms, and soles
Possible Viral Causes and Duration
The exact cause remains unclear, but evidence suggests:
- Association with human herpesvirus 6 (HHV-6) and HHV-7 reactivation
- Possible relation to other viral infections
- Potential genetic predisposition
- Not contagious from person to person in most cases
The condition follows a predictable timeline:
- Herald patch: Days 1-14
- Secondary eruption: Days 14-21
- Gradual fading: Weeks 4-8
- Potential post-inflammatory hyperpigmentation: May persist for months
Symptom Relief and Recovery
While pityriasis rosea resolves without treatment, symptom management includes:
- For itching (affects 25-75% of patients):
- Lukewarm baths with colloidal oatmeal
- Over-the-counter antihistamines (cetirizine, loratadine)
- Low to medium-potency topical corticosteroids for severe cases
- General measures:
- Avoid hot showers and baths (heat can worsen itching)
- Wear soft, breathable fabrics
- Apply moisturizers to prevent excessive dryness
- Limited sun exposure may help (though can worsen hyperpigmentation in darker skin)
- Medical intervention (for severe or persistent cases):
- Oral antihistamines
- Narrow-band UVB phototherapy
- Macrolide antibiotics (controversial benefit)
- Antiviral medications in selected cases
Rosacea
Rosacea is a chronic inflammatory skin condition affecting approximately 5% of the worldwide population, predominantly fair-skinned individuals of Northern European descent. This condition typically begins after age 30 and affects women more frequently, though men often experience more severe symptoms.

Facial Redness and Symptoms
Rosacea presents with characteristic features that may include:
- Persistent erythema (redness) of central face, particularly cheeks, nose, chin, and central forehead
- Flushing episodes that last longer than normal
- Telangiectasia (visible blood vessels near skin surface)
- Papules and pustules resembling acne but without comedones (blackheads/whiteheads)
- Phymatous changes (skin thickening and nodularity), especially of the nose (rhinophyma)
- Ocular symptoms in 50-72% of patients:
- Dry eyes, burning, or stinging
- Foreign body sensation
- Blepharitis (eyelid inflammation)
Triggers and Progressive Nature
Rosacea is believed to result from neurovascular dysregulation and innate immune system dysfunction. Common triggers include:
- Environmental factors:
- Sun exposure (UV radiation)
- Extreme temperatures (hot or cold)
- Wind exposure
- Dietary triggers:
- Spicy foods
- Hot beverages
- Alcohol (especially red wine)
- Foods containing cinnamaldehyde (tomatoes, citrus, chocolate)
- Other factors:
- Emotional stress
- Exercise
- Certain skincare products
- Medications that dilate blood vessels
- Demodex folliculorum mites (may play a role)
Without treatment, rosacea typically progresses through increasingly severe stages over time.
Skincare Approaches and Trigger Avoidance
Effective rosacea management combines:
- Gentle skincare routine:
- Mild, soap-free, pH-balanced cleansers
- Lukewarm water (avoid hot water)
- Pat dry instead of rubbing
- Wait 30 minutes after washing before applying medications
- Fragrance-free moisturizers with minimal ingredients
- Sun protection:
- Daily broad-spectrum SPF 30+ sunscreen
- Physical/mineral sunscreens (zinc oxide, titanium dioxide) preferred
- Wearing hats and seeking shade
- Medical treatments:
- Topical: metronidazole, azelaic acid, ivermectin, brimonidine
- Oral: antibiotics (doxycycline at anti-inflammatory doses), isotretinoin for severe cases
- Laser or intense pulsed light therapy for vascular symptoms
- Lifestyle adjustments:
- Keeping a trigger diary
- Stress management techniques
- Using green-tinted makeup to neutralize redness
Impetigo
Impetigo is a highly contagious bacterial skin infection primarily affecting children ages 2-5, though it can occur at any age. It’s one of the most common skin infections globally, particularly in warm, humid climates and crowded conditions.
Honey-Crusted Sores and Appearance
Impetigo presents in two main forms:
- Non-bullous impetigo (70% of cases):
- Begins as small red papules that rapidly evolve into vesicles or pustules
- Vesicles rupture easily, leaving erosions that ooze and develop honey-colored crusts
- Typically affects face (especially around nose and mouth) and extremities
- Lesions may be pruritic but rarely painful
- Resolves without scarring though temporary post-inflammatory hyperpigmentation may occur
- Bullous impetigo:
- Characterized by flaccid, transparent bullae (fluid-filled blisters) 1-2cm in diameter
- Filled with clear yellow fluid that darkens and becomes cloudy
- Rupture leaves behind thin, varnish-like coating
- Predominantly affects trunk, axillae, and groin folds
- Often asymptomatic apart from occasional mild burning sensation
Bacterial Causes and Contagious Nature
Impetigo is caused by:
- Staphylococcus aureus (most common in both forms)
- Streptococcus pyogenes (group A beta-hemolytic streptococci) alone or in combination with S. aureus
Transmission occurs through:
- Direct contact with lesions
- Contact with nasal carriers
- Touching contaminated objects
- Autoinoculation (spreading from one body area to another)
Risk factors include:
- Minor skin trauma (cuts, insect bites, eczema)
- Crowded living conditions
- Poor hygiene
- Warm, humid climate
- Compromised skin barrier (atopic dermatitis, scabies)
Treatment Needs and Preventing Spread
Effective management includes:
- Treatment approaches:
- Topical antibiotics (mupirocin, retapamulin) for limited disease
- Oral antibiotics for widespread or bullous impetigo:
- First-generation cephalosporins
- Clindamycin
- Amoxicillin-clavulanate
- Gentle removal of crusts with warm compresses before applying topical antibiotics
- Preventing spread:
- Washing hands frequently, especially after touching affected areas
- Using separate towels and linens for infected individuals
- Washing the patient’s clothes, towels, and bedding daily in hot water
- Keeping nails short and clean
- Avoiding close contact activities until 24-48 hours after starting treatment
- Covering lesions with loose bandages if returning to school/work
- When to seek additional care:
- Fever or systemic symptoms
- Lesions spreading despite treatment
- Signs of deeper infection (increased pain, redness, swelling)
- No improvement after 3 days of treatment
Scabies
Scabies is a highly contagious parasitic skin infestation caused by the microscopic mite Sarcoptes scabiei var. hominis. This condition affects approximately 300 million people globally each year, crossing all socioeconomic boundaries.
Intense Itching and Burrow Lines
Scabies presents with distinctive clinical features:
- Pruritus (itching):
- Intense, often worse at night and with heat
- Out of proportion to visible skin findings
- Typically begins 4-6 weeks after initial infestation (allergic hypersensitivity reaction to mites)
- Develops within 1-4 days in previously sensitized individuals
- Characteristic skin lesions:
- Burrows: Thread-like, grayish, slightly raised irregular lines 2-10mm long
- Papules: Small, erythematous, excoriated bumps
- Vesicles: Particularly on finger webs and wrists
- Nodules: Reddish-brown, pruritic nodules (10% of cases), often in genital areas
Typical distribution includes:
- Finger webs and sides of fingers
- Wrists and elbows (flexor surfaces)
- Axillary folds
- Belt line and buttocks
- Genital areas in men
- Periareolar region in women
In infants and young children, the head, neck, palms, and soles may also be affected.
Parasitic Mite Infestation Process
The scabies lifecycle and infestation process involves:
- Female mites (0.3-0.4mm) burrow into the stratum corneum (outermost skin layer)
- They deposit 2-3 eggs daily while creating burrows up to 5mm daily
- Eggs hatch into larvae after 3-4 days
- Larvae mature into adults, mate, and females create new burrows
- The entire lifecycle takes approximately 14 days
- Human hosts typically harbor 10-15 adult female mites
Crusted (Norwegian) scabies is a severe variant in immunocompromised individuals, characterized by thousands to millions of mites and highly contagious thick crusts.
Medical Treatment and Household Decontamination
Effective scabies management requires:
- Medical treatments:
- Permethrin 5% cream (first-line): Apply from neck down, leave for 8-14 hours, repeat in 7 days
- Ivermectin (oral): Particularly for crusted scabies or treatment failures, dosed at 200?g/kg, repeated in 7-14 days
- Alternative topicals: Crotamiton, sulfur preparations, benzyl benzoate
- Symptom management:
- Antihistamines for itching (may persist 2-4 weeks after successful treatment)
- Topical steroids for severe inflammation
- Antibiotics if secondary bacterial infection present
- Household/close contact management:
- Treat all household members and close physical contacts simultaneously, regardless of symptoms
- Wash clothing, bedding, and towels in hot water (?60°C) and dry at high heat
- Items that cannot be washed should be sealed in plastic bags for 72 hours
- Vacuum furniture and carpets (mites survive only 2-3 days off human skin)
- Institutional outbreaks:
- Require coordinated treatment of all potentially exposed individuals
- Implementation of contact precautions
- Environmental cleaning protocols
Shingles (Herpes Zoster)
Shingles, or herpes zoster, results from reactivation of the varicella-zoster virus (VZV), which lies dormant in sensory nerve ganglia following chickenpox infection. This painful condition affects approximately 1 in 3 people during their lifetime, with incidence increasing dramatically after age 50.
Painful Band of Blisters and Nerve Pain
Shingles presents with a distinct clinical progression:
- Prodromal phase (1-5 days before rash):
- Burning, tingling, or shooting pain in a dermatomal distribution
- Itching or numbness in affected area
- Occasional fever, headache, and malaise
- Acute eruptive phase:
- Erythematous, grouped vesicles on an inflamed base
- Unilateral distribution following one or adjacent dermatomes
- Most commonly affects thoracic (50-60%), cervical (10-20%), or trigeminal (10-20%, particularly ophthalmic) dermatomes
- Vesicles evolve to pustules, then crust over within 7-10 days
- Complete healing typically occurs within 2-4 weeks
The pain of shingles is often described as:
- Burning, stabbing, or electric-shock-like
- Constant or intermittent
- Potentially exacerbated by light touch (allodynia)
- More severe in older adults
Reactivated Chickenpox Virus Explanation
Shingles pathophysiology involves:
- Primary VZV infection (chickenpox) establishing latency in dorsal root or cranial nerve ganglia
- Virus maintained in latency by VZV-specific cell-mediated immunity
- Reactivation occurring when immunity wanes (aging) or is compromised
- Reactivated virus traveling down sensory nerve to skin, causing inflammation and vesicle formation
Risk factors for reactivation include:
- Age over 50 (declining cell-mediated immunity)
- Immunosuppression (medications, diseases like HIV)
- Recent trauma or stress
- Radiotherapy
- Systemic diseases (diabetes mellitus, rheumatoid arthritis)
Early Intervention and Pain Management
Optimal shingles management includes:
- Antiviral therapy (most effective when started within 72 hours of rash onset):
- Acyclovir, valacyclovir, or famciclovir
- Reduces viral shedding, lesion formation, and acute pain
- May decrease risk of postherpetic neuralgia
- Pain management strategies:
- Analgesics: Acetaminophen, NSAIDs for mild pain
- Neuropathic pain medications: Gabapentin, pregabalin, tricyclic antidepressants
- Short-term opioids for severe pain
- Topical therapies: Lidocaine patches, capsaicin cream
- Nerve blocks in selected cases
- Supportive care:
- Cool compresses to reduce pain and itching
- Calamine lotion for itching
- Keeping lesions clean to prevent secondary infection
- Loose-fitting clothing to minimize friction
- Prevention:
- Recombinant zoster vaccine (Shingrix) recommended for adults 50+ and immunocompromised adults 19+
- 90% effective in preventing shingles and postherpetic neuralgia
Drug Rashes
Cutaneous drug reactions affect 2-3% of hospitalized patients and up to 1% of outpatients who take medications. These adverse reactions range from mild, self-limited eruptions to life-threatening conditions.
Various Presentation Patterns
Drug rashes exhibit diverse morphologies and distributions:
- Maculopapular (exanthematous) eruptions (most common, 75-90% of all cutaneous drug reactions):
- Symmetrically distributed pink-to-red macules and papules
- Often starts on trunk and spreads peripherally
- May become confluent
- Typically appears 7-14 days after starting new medication
- Urticarial reactions:
- Itchy, edematous, red wheals
- Individual lesions resolve within 24 hours
- Can appear minutes to hours after drug exposure
- Fixed drug eruptions:
- Solitary or multiple round, well-demarcated plaques
- Reddish-purple to brown color
- Recur at same site with re-exposure to causative drug
- Resolve with post-inflammatory hyperpigmentation
- Photosensitivity reactions:
- Exaggerated sunburn or eczematous reaction in sun-exposed areas
- Can be phototoxic (direct tissue damage) or photoallergic (immune-mediated)
- Severe cutaneous adverse reactions (SCARs – medical emergencies):
- Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis: Widespread blistering and mucosal involvement
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS): Extensive rash, fever, internal organ involvement
- Acute Generalized Exanthematous Pustulosis (AGEP): Widespread small sterile pustules
Common Medication Triggers
While any medication can potentially cause a reaction, common offenders include:
- Antibiotics:
- Beta-lactams (penicillins, cephalosporins)
- Sulfonamides
- Fluoroquinolones
- Macrolides
- Anticonvulsants:
- Carbamazepine
- Phenytoin
- Lamotrigine
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Allopurinol
- Biological agents
- Contrast media
- Chemotherapeutic agents
Certain medications have characteristic reaction patterns and genetic predispositions that increase risk.
Management and Medication History Importance
Effective management of drug rashes requires:
- Accurate diagnosis:
- Detailed medication history, including prescription, over-the-counter, supplements
- Timing of drug initiation relative to rash onset
- Previous medication reactions
- Characteristic patterns associated with specific drugs
- Immediate intervention:
- Discontinuation of suspected causative agent(s)
- Emergency care for severe reactions (SCARs)
- Supportive care based on symptoms
- Symptomatic treatment:
- Antihistamines for itching
- Topical corticosteroids for inflammation
- Moisturizers for dryness and comfort
- Tepid baths with colloidal oatmeal
- Documentation and future prevention:
- Clear documentation of reaction in medical records
- Patient education regarding medications to avoid
- Medical alert identification in severe cases
- Consider testing (patch testing, genetic testing) in selected cases
- Cross-reactivity awareness (e.g., among beta-lactams or NSAIDs)
Conclusion
Understanding the distinctive characteristics of common skin rashes is essential for appropriate care and knowing when to seek medical attention. While many rashes can be safely managed at home, others require prompt professional intervention to prevent complications.
Key identification features to remember include:
- Distribution pattern (symmetrical, dermatomal, or localized)
- Morphology (papules, vesicles, plaques, or scales)
- Associated symptoms (itching, pain, or burning)
- Timing and progression
- Potential triggers or exposures
General skin care principles that help prevent many rashes include:
- Gentle cleansing with mild, fragrance-free products
- Regular moisturizing, especially after bathing
- Avoiding known irritants and allergens
- Wearing protective clothing when appropriate
- Sun protection with broad-spectrum SPF
- Maintaining good hand hygiene
Consult healthcare providers promptly when rashes:
- Are accompanied by fever, pain, or signs of infection
- Develop suddenly and spread rapidly
- Involve blistering, especially around mucous membranes
- Don’t improve with appropriate home care
- Recur frequently or worsen over time
- Affect daily activities or quality of life
For further information about skin conditions, reliable resources include the American Academy of Dermatology (aad.org), National Eczema Association (nationaleczema.org), and dermatology departments of major medical institutions, which often provide educational materials about common skin conditions.

