Your heart rate is more than just a number – it’s a vital sign that can provide critical clues about your cardiovascular health. While occasional fluctuations are normal, certain heart rate patterns can signal serious underlying conditions that require immediate medical attention. Recognizing these warning signs could be life-saving, especially if you or someone you love is experiencing unusual heart activity.
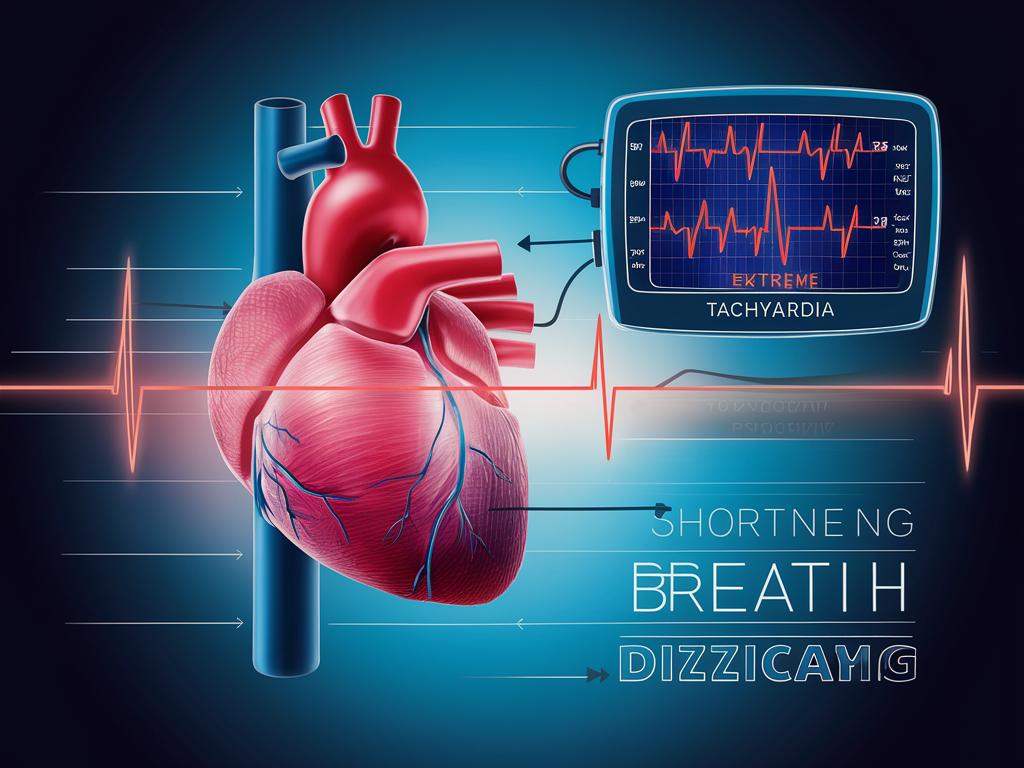
1. Extreme Tachycardia (Abnormally Fast Heart Rate)
Tachycardia occurs when your heart consistently beats faster than normal while at rest. For adults, a resting heart rate above 100 beats per minute (BPM) is considered tachycardia, but it becomes particularly concerning when it exceeds 120-140 BPM without physical exertion.
When your heart races this rapidly without cause, you may experience:
- Shortness of breath or difficulty breathing
- Chest pain or discomfort
- Lightheadedness or dizziness
- A sensation of your heart “pounding” in your chest
Several factors can trigger dangerous tachycardia, including excessive caffeine consumption, certain medications, anxiety, and underlying heart conditions such as coronary artery disease or heart valve problems. Medical conditions like hyperthyroidism, anemia, and infection can also cause an abnormally rapid heart rate.
If you experience persistent tachycardia with symptoms, especially chest pain or difficulty breathing, seek emergency medical attention immediately.
2. Severe Bradycardia (Abnormally Slow Heart Rate)
Bradycardia is defined as a heart rate below 60 BPM in non-athletes. While well-conditioned athletes often have naturally lower heart rates, bradycardia in others can indicate a problem with the heart’s electrical system.
Bradycardia becomes dangerous when your heart rate drops below 40 BPM and is accompanied by symptoms such as:
- Extreme fatigue or constant tiredness
- Weakness and reduced exercise capacity
- Near-fainting or fainting episodes (syncope)
- Confusion or difficulty concentrating
- Shortness of breath, especially during mild activity
Elderly individuals and those with pre-existing heart conditions are at higher risk for dangerous bradycardia. Causes can include aging-related changes in heart tissue, heart disease, hypothyroidism, electrolyte imbalances, and side effects from medications like beta-blockers and certain antiarrhythmics.
Severe bradycardia may require a pacemaker to maintain a heart rate sufficient to sustain normal cardiac output and prevent organ damage.
3. Heart Palpitations That Don’t Resolve
Heart palpitations—sensations of skipped beats, fluttering, or pounding in your chest—are fairly common and often harmless. However, they can signal a dangerous condition when they persist for extended periods or recur frequently.
Potentially dangerous palpitations typically:
- Last more than a few minutes
- Occur repeatedly over short periods
- Are accompanied by chest pain, severe dizziness, or fainting
- Worsen over time rather than improve
While brief palpitations from stress or caffeine are usually benign, persistent palpitations may indicate arrhythmias like atrial fibrillation or ventricular tachycardia. They can also signal structural heart problems such as valve disorders or cardiomyopathy.
When palpitations occur with shortness of breath, chest pain, severe dizziness, or fainting, it’s crucial to seek immediate medical attention as these could indicate a life-threatening cardiac event.
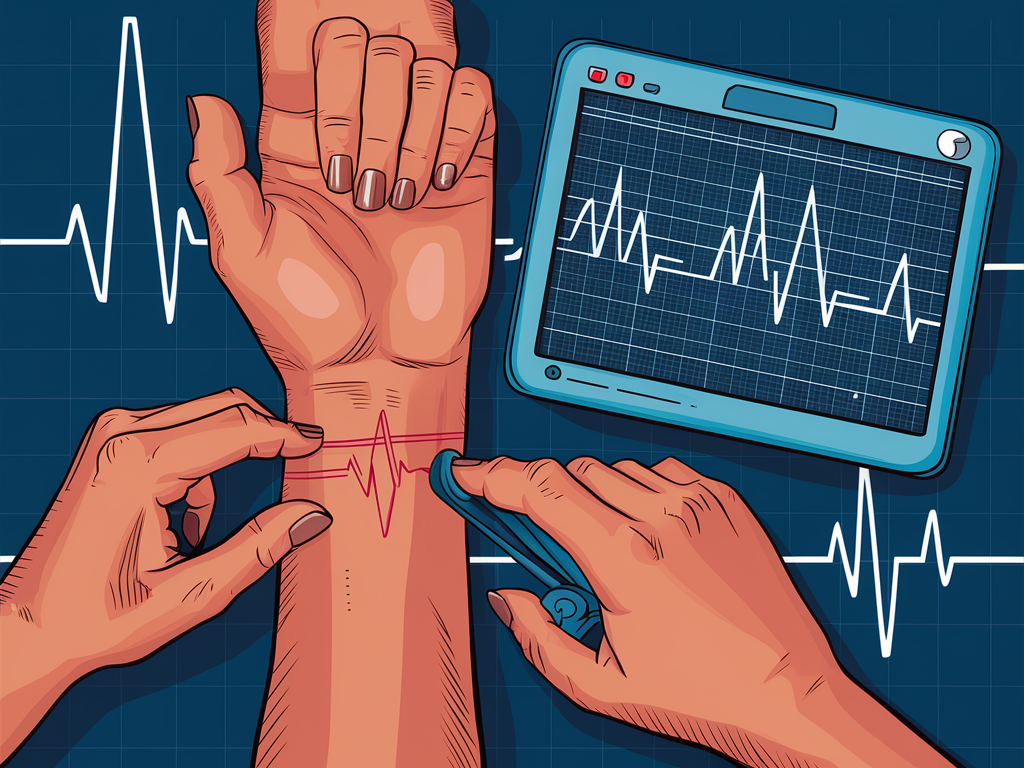
4. Irregular Heart Rhythm (Arrhythmia)
An irregular heart rhythm, or arrhythmia, occurs when the electrical impulses coordinating your heartbeats don’t function properly. While some arrhythmias are harmless, others can be life-threatening.
Dangerous arrhythmias include:
- Atrial fibrillation – characterized by chaotic, rapid electrical signals in the upper chambers
- Ventricular tachycardia – a rapid heart rhythm originating in the heart’s lower chambers
- Ventricular fibrillation – a chaotic heart rhythm that can lead to cardiac arrest
You can self-check for irregular rhythms by feeling your pulse at your wrist or neck. A healthy heart beats with a steady, consistent rhythm. If you notice irregular patterns—skipped beats, extra beats, or completely chaotic rhythms—it may indicate an arrhythmia.
Red flags that indicate a medical emergency include irregular heart rhythms accompanied by:
- Chest pain or pressure
- Difficulty breathing
- Severe dizziness or fainting
- Confusion or altered mental status
5. Sudden Changes in Heart Rate Without Obvious Cause
Your heart rate naturally fluctuates throughout the day in response to activity, emotions, and environmental factors. However, sudden, dramatic changes without an identifiable trigger warrant attention.
Concerning patterns include:
- Rapid acceleration of heart rate while at rest
- Sudden drops in heart rate not associated with relaxation
- Heart rate that jumps between extremes within short periods
These sudden shifts may indicate autonomic nervous system dysfunction, where the mechanisms controlling involuntary body functions aren’t working properly. This can occur in conditions like postural orthostatic tachycardia syndrome (POTS) or autonomic neuropathy.
Medications can also cause dangerous heart rate fluctuations as side effects. Drugs that may affect heart rate stability include stimulants, certain antidepressants, and some blood pressure medications when dosing isn’t optimized.
6. Heart Rate That Doesn’t Respond Appropriately to Activity
A healthy heart increases its rate during physical activity and returns to baseline within a few minutes after exertion ends. When this normal response is absent, it may signal cardiovascular problems.
Two important warning signs to monitor:
- Insufficient increase during exertion: Your heart rate should increase in proportion to exercise intensity. If your heart rate barely rises despite significant physical effort, this could indicate “chronotropic incompetence”—the heart’s inability to accelerate appropriately.
- Failure to return to baseline: After exercise, your heart rate should gradually return to your resting rate. If it remains elevated for more than 10-15 minutes post-exercise, this could suggest poor cardiovascular fitness or underlying heart problems.
Chronotropic incompetence often indicates issues with the heart’s electrical conduction system, possible coronary artery disease, or heart failure. This condition significantly reduces exercise capacity and quality of life, and can increase mortality risk if left untreated.
7. Extreme Heart Rate Variability
Heart rate variability (HRV)—the variation in time between consecutive heartbeats—is actually a positive indicator of cardiovascular health when present in moderate amounts. However, extreme variability can signal dangerous conditions.
Unhealthy heart rate variability presents as:
- Dramatic swings between very fast and very slow rates without apparent cause
- Irregular patterns that feel chaotic rather than rhythmic
- Heart rate that seems to “pause” momentarily before resuming
Sick sinus syndrome, a condition where the heart’s natural pacemaker (sinus node) malfunctions, often manifests as extreme heart rate variability. Affected individuals may experience alternating episodes of bradycardia and tachycardia, known as “tachy-brady syndrome.”
Modern wearable devices and smartphone apps can help monitor HRV, but medical-grade monitoring is necessary for accurate diagnosis. If you notice extreme irregularity in your heart rate, particularly if accompanied by symptoms, consult a healthcare provider promptly.
8. Nocturnal Tachycardia (Elevated Heart Rate During Sleep)
During normal sleep, your heart rate typically slows, averaging between 40-60 BPM, reflecting the rest-and-repair stage of your body. A consistently elevated heart rate during sleep, especially above 90 BPM, is abnormal and concerning.
Nocturnal tachycardia is particularly worrisome because:
- It indicates your cardiovascular system isn’t getting proper rest
- It’s associated with increased stress hormone production
- It can contribute to insomnia and poor sleep quality
- It may signal serious conditions requiring intervention
This condition frequently occurs with sleep apnea, a disorder where breathing repeatedly stops and starts during sleep. The oxygen deprivation triggers heart rate increases as your body tries to compensate. Untreated sleep apnea significantly increases cardiovascular disease risk.
Other causes include anxiety disorders, hyperthyroidism, and certain medications. Monitoring can be done through smartwatches, dedicated sleep trackers, or medical sleep studies. If your sleeping heart rate consistently exceeds 90 BPM or you experience night sweats, shortness of breath while sleeping, or extreme fatigue despite adequate sleep, consult a healthcare provider.
9. Heart Rate Changes Accompanied by Syncope (Fainting)
Fainting (syncope) that occurs alongside heart rate abnormalities often indicates serious cardiac problems. This combination happens because inadequate heart function leads to insufficient blood flow to the brain.
Watch for these pre-syncope warning signs:
- Sudden lightheadedness or dizziness
- Blurred vision or tunnel vision
- Cold sweat and pallor
- Nausea
- Feeling that your heart is racing, pounding, or skipping beats

Cardiac syncope differs from other fainting causes (like vasovagal syncope) because it:
- Often occurs with minimal warning
- Can happen during physical activity rather than just in response to triggers like pain or stress
- May be preceded by palpitations or chest discomfort
- Carries a higher risk of injury and recurrence
If syncope occurs with heart rate changes, call emergency services immediately. Until help arrives, place the person in the recovery position (on their side) to maintain an open airway and prevent aspiration if vomiting occurs.
10. Persistent Heart Rate Changes with Systemic Symptoms
When heart rate abnormalities occur alongside systemic symptoms affecting the whole body, this often indicates that either the heart problem is affecting multiple organ systems, or a systemic condition is affecting the heart.
Be vigilant for these combinations:
- Persistent tachycardia with fever, fatigue, and unexplained weight loss
- Bradycardia with cold intolerance, constipation, and weight gain
- Heart rhythm changes with joint pain, rashes, and persistent fever
These constellations of symptoms may point to conditions like:
- Thyroid disorders (hyperthyroidism causing tachycardia; hypothyroidism causing bradycardia)
- Systemic infections and sepsis
- Autoimmune diseases affecting the heart (like lupus or rheumatic fever)
- Infiltrative diseases (like sarcoidosis or amyloidosis)
Comprehensive evaluation is essential in these cases and may include blood tests, imaging studies, and specialty consultations. Because these conditions affect multiple body systems, an interdisciplinary approach is often needed for proper diagnosis and treatment.
When to Seek Emergency Medical Attention
Don’t hesitate to call emergency services if you experience:
- Heart rate above 120 BPM while at rest with chest pain or difficulty breathing
- Heart rate below 40 BPM with dizziness, weakness, or confusion
- Irregular heartbeats with fainting or near-fainting
- Heart palpitations with chest pain that radiates to the jaw, arm, or back
- Any heart rate abnormality with severe shortness of breath or profound fatigue
Understanding these warning signs and seeking timely medical intervention can be life-saving. Remember that heart rate abnormalities often provide early warning of serious cardiovascular issues before more severe complications develop.
Regular check-ups, appropriate monitoring for those with known risk factors, and prompt attention to new or worsening symptoms are essential components of heart health maintenance. When in doubt about heart rate changes, especially when accompanied by other concerning symptoms, it’s always better to err on the side of caution and seek medical evaluation.

