Facial degloving represents one of the most severe traumatic injuries in maxillofacial trauma medicine. This catastrophic injury occurs when the facial soft tissues become separated from the underlying bone structures, creating devastating consequences for both function and appearance. Understanding this condition is crucial for medical professionals, high-risk individuals, and anyone who may witness such an emergency situation.
Fact #1: Understanding the Mechanism of Facial Degloving
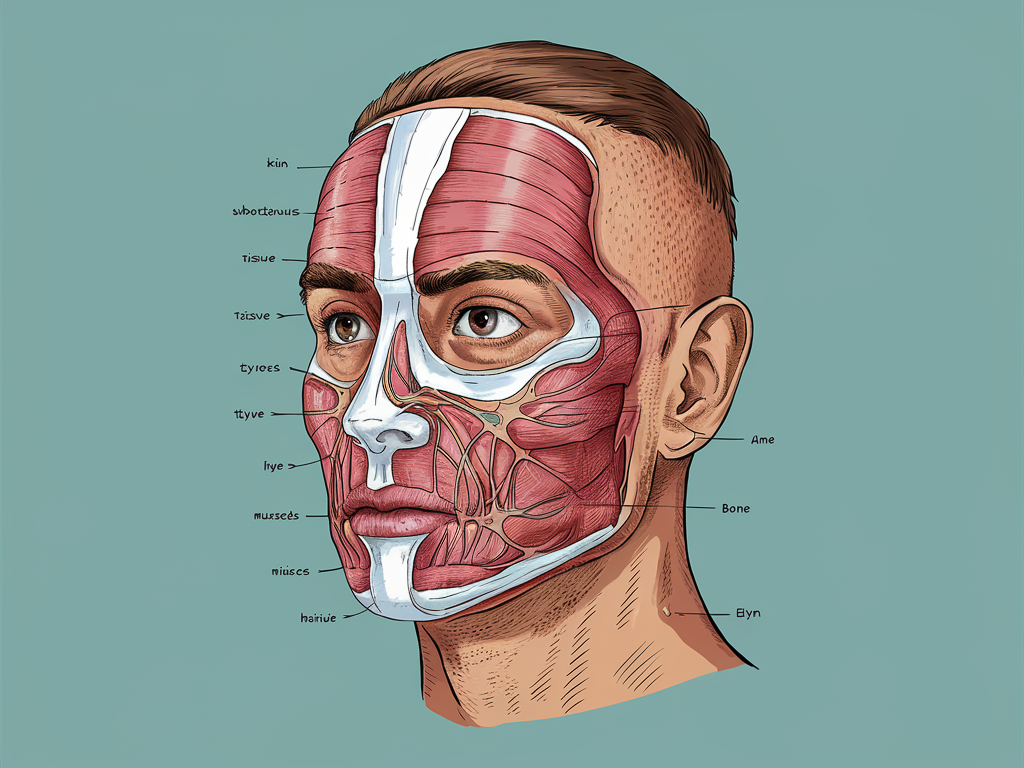
Facial degloving involves the traumatic avulsion of facial soft tissues from their underlying bony attachments. Unlike lacerations or fractures, degloving specifically refers to the separation of large areas of skin, subcutaneous tissue, and sometimes deeper structures from the facial skeleton. This occurs when significant shearing forces are applied to the face, creating a plane of separation between tissue layers.
The injury typically affects multiple facial regions simultaneously, including:
- Periorbital tissues surrounding the eyes
- Nasolabial regions around the nose and mouth
- Cheek and maxillary areas
- Perioral tissues surrounding the lips
- Submental and submandibular regions below the chin
What distinguishes degloving from other facial traumas is the extensive nature of tissue separation rather than individual structural damage. The facial soft tissue envelope essentially “peels away” from the facial skeleton, damaging critical neurovascular structures in the process.
Fact #2: Primary Causes of Facial Degloving Injuries
Facial degloving injuries result from extreme forces that create shearing pressure against facial tissues. The most common causes include:
Motor Vehicle Accidents
Automobile and motorcycle collisions represent the leading cause of facial degloving, particularly when:
- Unrestrained occupants impact the dashboard or windshield
- Motorcyclists or cyclists experience “road rash” against pavement
- Airbag deployment creates forceful lateral pressure
- Steering wheel impact occurs during frontal collisions
Industrial Accidents
Workplace incidents involving heavy machinery pose significant risks, particularly:
- Entanglement in rotating equipment or conveyor belts
- Compression injuries between heavy objects
- High-pressure injection injuries
- Construction site falls with facial impact
Falls From Significant Heights
Vertical drops exceeding 10-15 feet frequently result in facial impact with:
- Lateral shearing forces upon impact
- Acceleration-deceleration mechanisms
- Multiple impact points during the fall
Animal Attacks
Large animal bites, particularly from dogs, can create degloving by:
- Bite-and-pull mechanisms tearing tissue from bone
- Clawing actions that penetrate and separate tissue planes
- Crush injuries from powerful jaw pressure
Sports-Related Trauma
High-velocity sports carry degloving risks through:
- Direct facial impacts in contact sports
- Equipment-related injuries (such as hockey sticks or balls)
- Falls onto hard surfaces during extreme sports
- Water sports accidents with high-speed water impact
Fact #3: Warning Signs and Immediate Symptoms
Facial degloving presents with unmistakable and severe clinical manifestations that demand immediate medical intervention. Recognizing these critical signs can expedite appropriate emergency response:
Visible Tissue Separation
The most obvious sign is extensive soft tissue detachment, with:
- Hanging or mobile facial tissue segments
- Exposed underlying facial bones
- Visible separation between skin and deeper structures
- Abnormal tissue mobility when gently touched
Severe Facial Deformity
The face shows dramatic distortion including:
- Abnormal facial contours and proportions
- Displaced facial features (nose, lips, cheeks)
- Asymmetry beyond what typical facial trauma creates
- Sunken areas where tissue support is lost
Massive Hemorrhage
Extensive bleeding occurs due to:
- Disruption of facial arteries and veins
- Multiple bleeding points across extensive surface areas
- Continuous blood loss resistant to direct pressure
- Blood pooling in detached tissue spaces
Neurosensory Deficits
Patients experience profound sensory abnormalities:
- Complete loss of sensation in affected facial regions
- Inability to detect touch, temperature, or pain
- Numbness following distribution patterns of facial nerves
- Paresthesia (tingling or “pins and needles” sensations)
Facial Movement Impairment
Motor function becomes compromised through:
- Inability to form facial expressions
- Paralysis of specific facial muscle groups
- Mechanical limitation from tissue displacement
- Asymmetrical movement during attempts at expression
Fact #4: Emergency Response for Facial Degloving
The immediate response to facial degloving can significantly impact survival and long-term outcomes. Critical emergency interventions include:
Immediate First Aid
- Establish and maintain a patent airway as the absolute priority
- Control hemorrhage through direct pressure to bleeding vessels
- Preserve avulsed tissue by gently repositioning without tension
- Irrigate exposed tissues with sterile saline if available
- Cover exposed areas with clean, moist dressings
Critical Do’s and Don’ts
Do:
- Support the patient’s neck in case of concurrent cervical injury
- Keep the patient warm to prevent hypothermia
- Collect and properly preserve any completely separated tissue
- Document the time of injury and mechanism
- Monitor vital signs continuously
Don’t:
- Attempt to clean severely contaminated wounds with anything but sterile solution
- Remove foreign objects embedded in the wounds
- Apply antiseptic solutions to exposed bone or muscle
- Allow degloved tissue to dry out
- Delay transport to definitive care
Transport Considerations
Rapid transfer to appropriate facilities is essential:
- Transport directly to a Level I trauma center when possible
- Alert receiving facility about the specific nature of injuries
- Maintain tissue viability during transport with proper wound care
- Position the patient to prevent aspiration of blood
- Provide advanced life support measures throughout transport
Fact #5: Diagnostic Procedures for Facial Degloving
Accurate assessment of facial degloving requires comprehensive diagnostic evaluation through multiple modalities:
Initial Clinical Assessment
Emergency providers perform rapid evaluation focusing on:
- Airway patency and respiratory function
- Hemodynamic stability and blood loss estimation
- Neurological status including Glasgow Coma Scale
- Visual assessment of tissue viability (color, capillary refill)
- Manual examination of bone stability and step-offs
Advanced Imaging
Critical imaging studies include:
- CT Scanning: The gold standard for evaluating both bony and soft tissue injuries with 3D reconstruction capabilities
- CT Angiography: Identifies vascular injuries, particularly to facial and carotid arteries
- MRI: Used selectively for detailed soft tissue evaluation after stabilization
- Doppler Ultrasound: Bedside assessment of blood flow in questionable areas
- Panoramic Radiography: May assist in evaluating mandibular integrity
Tissue Viability Assessment
Determining tissue salvageability involves:
- Fluorescein dye studies to assess microcirculation
- Near-infrared spectroscopy to measure tissue oxygenation
- Clinical assessment of tissue color, temperature, and capillary refill
- Evaluation of bleeding upon surgical debridement
- Intraoperative assessment of muscle contractility
Fact #6: Treatment Approaches and Surgical Interventions
Management of facial degloving requires a complex, multidisciplinary approach with staged interventions:
Emergency Surgical Procedures
Initial surgeries focus on:
- Securing the airway through intubation or tracheostomy
- Hemostasis and vascular control of major bleeding sources
- Thorough debridement of nonviable tissue
- Temporary wound closure techniques
- Skeletal fixation of associated facial fractures
Tissue Preservation Strategies
Maintaining tissue viability requires:
- Revascularization through microvascular repair of identifiable vessels
- Tension-free reapproximation of degloved tissues
- Placement of surgical drains to prevent hematoma formation
- Application of negative pressure wound therapy in some cases
- Hyperbaric oxygen therapy consideration for compromised tissues
Reconstructive Surgery Options
Later stage procedures may include:
- Free tissue transfer using microsurgical techniques
- Local and regional flap reconstruction
- Facial reanimation procedures for nerve injuries
- Secondary skeletal contouring and augmentation
- Scar revision and surface treatments
Multidisciplinary Care Team
Comprehensive treatment involves coordination among:
- Trauma surgeons and emergency physicians
- Oral and maxillofacial surgeons
- Plastic and reconstructive surgeons
- Otolaryngologists (ENT specialists)
- Ophthalmologists for orbital involvement
- Neurosurgeons for cranial extensions
- Specialist nursing and rehabilitation professionals
Fact #7: Recovery Process and Timeline
The rehabilitation journey after facial degloving is prolonged and complex, typically spanning months to years:
Initial Healing Phase (0-6 weeks)
- Acute wound healing and monitoring for complications
- Management of edema through positioning and compression
- Pain control and prevention of wound contraction
- Nutritional support often requiring alternative feeding methods
- Protection of healing tissues from external pressure or trauma
Intermediate Recovery (6 weeks to 6 months)
- Progressive tissue remodeling and scar maturation
- Initiation of gentle facial exercises
- Staged reconstructive procedures as tissues stabilize
- Early intervention for contractures or adhesions
- Transition to oral nutrition and speech rehabilitation
Long-term Rehabilitation (6 months onward)
- Intensive physical therapy targeting facial musculature
- Neuromuscular retraining for facial expression
- Scar management through massage, silicone therapy, and laser treatments
- Secondary refinement surgeries for aesthetic improvement
- Adaptive strategies for permanent functional limitations
Psychological Support
Mental health interventions are crucial and include:
- Trauma-focused cognitive behavioral therapy
- Body image counseling and adjustment therapy
- Support groups and peer connections
- Family therapy to address relationship changes
- Vocational rehabilitation and social reintegration support
Fact #8: Potential Complications and Long-term Effects
Facial degloving carries significant risks for ongoing complications and permanent sequelae:
Functional Impairments
- Oral incompetence affecting eating, drinking, and saliva control
- Nasal airway obstruction and breathing difficulties
- Malocclusion and mastication problems
- Speech articulation disorders
- Lacrimal system dysfunction causing dry eye or excessive tearing
Aesthetic Considerations
- Facial asymmetry and contour irregularities
- Hypertrophic or keloid scarring
- Tissue atrophy and volume deficiency
- Color and texture mismatch between reconstructed areas
- Visible deformities affecting social interaction
Neurological Sequelae
- Permanent facial nerve paralysis or paresis
- Trigeminal nerve injury causing sensory deficits
- Neuropathic pain syndromes
- Autonomic dysfunction affecting sweating or vasomotor control
- Complex regional pain syndrome development
Psychological Impact
- Post-traumatic stress disorder (PTSD)
- Depression and anxiety disorders
- Social avoidance and isolation
- Body dysmorphic concerns
- Identity disruption and grief for pre-injury appearance

Fact #9: Risk Factors and High-Risk Populations
Certain demographics, occupations, and conditions increase vulnerability to facial degloving injuries:
Occupational Hazards
High-risk professions include:
- Construction workers: Exposed to falls, heavy machinery, and projectiles
- Manufacturing personnel: Working with rotating equipment and industrial presses
- Agricultural workers: At risk from farm machinery and large animal encounters
- Loggers and forestry workers: Facing dangers from falling objects and chainsaw accidents
- Mining industry employees: Subject to confined space injuries and equipment hazards
High-Risk Activities
- Motorsports and high-speed vehicle recreation
- Contact sports without adequate facial protection
- Extreme sports (downhill mountain biking, skateboarding, etc.)
- Handling large, potentially aggressive animals
- Activities involving exposed rotating machinery
Predisposing Medical Conditions
Pre-existing factors that may worsen outcomes include:
- Connective tissue disorders (Ehlers-Danlos syndrome, Marfan syndrome)
- Bleeding disorders or anticoagulant medication use
- Conditions affecting wound healing (diabetes, peripheral vascular disease)
- Immunocompromised states impairing infection resistance
- Prior facial surgeries creating planes of weakness
Age-Related Considerations
- Pediatric patients face unique challenges with growth and development
- Elderly individuals experience delayed healing and tissue friability
- Young adults show higher incidence due to risk-taking behaviors
- Middle-aged populations face occupational exposure risks
Fact #10: Prevention Strategies and Safety Measures
While some accidents cannot be prevented, many facial degloving injuries are potentially avoidable through proper safety measures:
Personal Protective Equipment
- Full-face shields for high-risk industrial operations
- Sport-specific facial protection (hockey cages, football face guards)
- Properly fitted helmets with face protection for motorsports
- Impact-resistant eyewear extending to cheek coverage
- Chin straps and mandibular protection for high-velocity activities
Workplace Safety Protocols
- Machine guarding for all rotating or moving equipment parts
- Lock-out/tag-out procedures during maintenance operations
- Proper training on equipment operation and emergency stops
- Fall protection systems for elevation work
- Regular safety audits and compliance monitoring
Vehicle Safety Enhancements
- Consistent seatbelt use and proper positioning
- Appropriate airbag systems with modern deployment technology
- Crumple zone engineering in vehicle design
- Enhanced windshield and side window safety standards
- Motorcycle/bicycle helmet use with full-face protection
Recreational Safety
- Sport-specific training on collision avoidance
- Proper technique instruction for high-risk activities
- Environmental assessment before participation
- Gradual progression in skill development
- Supervision for novice participants
Conclusion
Facial degloving represents one of the most devastating traumatic injuries affecting both form and function of the face. This comprehensive review has outlined the critical aspects of understanding, recognizing, treating, and preventing these life-altering injuries. The complexity of facial tissue architecture means that degloving injuries require specialized multidisciplinary care and extensive rehabilitation.
The immediate recognition of warning signs and appropriate emergency response significantly impacts survival and long-term outcomes. For those who experience such trauma, the recovery journey is challenging but advances in reconstructive techniques continue to improve functional and aesthetic results.
Prevention remains the most effective approach, particularly through proper safety equipment, workplace protocols, and risk awareness. For high-risk individuals, understanding the mechanisms and contexts in which these injuries occur provides valuable knowledge that may prevent life-changing trauma.
If you require additional information or support regarding facial trauma, consult with maxillofacial specialists, trauma centers, or facial injury support organizations that can provide resources tailored to your specific needs.

