Your bathroom visits might seem routine, but what you leave behind in the toilet bowl can reveal surprising insights about your overall health. The appearance, consistency, frequency, and color of your stool serve as valuable indicators of your digestive system’s functioning and can even signal underlying health conditions.
Healthcare professionals often use the Bristol Stool Chart as a clinical tool to classify human feces into seven categories based on shape and consistency. This classification helps identify potential digestive issues and guides treatment approaches.
Paying attention to your bowel movements isn’t just about noticing problems—it’s an essential practice for proactive health monitoring. Changes in your stool’s appearance may provide early warning signs of digestive disorders, nutritional imbalances, or more serious health concerns.
In this comprehensive guide, we’ll examine 15 different types of stool based on consistency, shape, and color. You’ll learn what constitutes healthy bowel movements, what changes might indicate, and when you should consult a healthcare provider. We’ve also included a visual color chart to help you better understand what your stool is telling you about your health.
Understanding Normal Stool
Before diving into the various types of stool, it’s important to establish what’s considered “normal.” Healthy bowel movements should be relatively easy to pass without straining, pain, or discomfort. They typically have a brown color, a soft but formed consistency, and a cylindrical or sausage-like shape.
When it comes to frequency, there’s considerable variation among individuals. While some people have bowel movements three times daily, others may go three times a week. Both patterns can be normal if they’re consistent for you and aren’t accompanied by discomfort or other concerning symptoms.
The ideal stool passes smoothly and completely, with a cohesive texture that isn’t too hard or too loose. It should sink slowly in the toilet water rather than floating or sinking immediately, and shouldn’t contain visible undigested food (except for certain high-fiber items like corn or seeds).
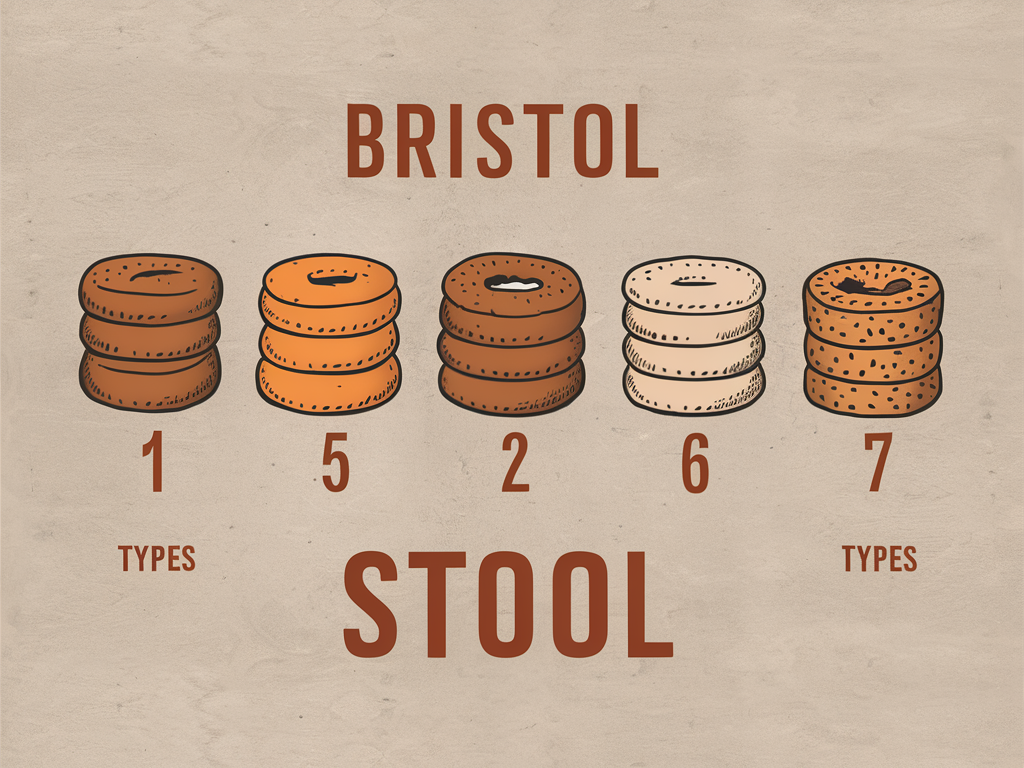
Types of Poop Based on Consistency and Shape
1. Type 1: Separate Hard Lumps (Severe Constipation)
Appearance and characteristics: Small, separate hard lumps that resemble nuts or rabbit pellets. These are difficult and often painful to pass.
Causes and contributing factors: Type 1 stools typically result from prolonged intestinal transit time, where waste moves too slowly through your colon. Common causes include dehydration, insufficient dietary fiber, sedentary lifestyle, certain medications (particularly opioids and some antidepressants), and ignoring the urge to defecate.
When to be concerned: Occasional Type 1 stools aren’t usually cause for alarm, but persistent occurrence may indicate chronic constipation. If you experience this stool type regularly alongside abdominal pain, bloating, or an inability to pass stool for several days, medical attention is warranted.
Remedies and prevention: Increase water intake to at least 8-10 glasses daily. Gradually incorporate more fiber-rich foods like fruits, vegetables, and whole grains. Regular physical activity stimulates intestinal contractions. Over-the-counter fiber supplements or stool softeners may help temporarily, but shouldn’t become a long-term solution without medical guidance.
2. Type 2: Sausage-Shaped but Lumpy (Mild Constipation)
Appearance and characteristics: Sausage-shaped but composed of lumps that are stuck together, resembling a cobblestone path or a bunch of grapes pressed together. These stools are still difficult to pass but less so than Type 1.
Causes and contributing factors: Similar to Type 1, but representing a less severe form of constipation. Often results from mild dehydration, inadequate fiber intake, or recent dietary changes. Stress and anxiety can also contribute by disrupting normal gut motility.
When to be concerned: If Type 2 stools persist for more than two weeks or are accompanied by unexplained weight loss, rectal bleeding, or severe abdominal pain, consult a healthcare provider.
Remedies and prevention: The interventions for Type 1 apply here as well. Additionally, establishing a regular bathroom routine can help—try to have bowel movements at approximately the same time each day. Warm liquids in the morning, particularly coffee, can stimulate bowel movements for many people.
3. Type 3: Sausage-Shaped with Cracks (Slightly Constipated)
Appearance and characteristics: Sausage-shaped but with surface cracks or fissures. These pass more easily than Types 1 and 2 but still indicate slight constipation.
Causes and contributing factors: Mild dehydration or slightly inadequate fiber intake. Often seen during transitional periods when improving diet or increasing fluid intake after previous constipation.
Remedies and prevention: Continue increasing water intake and dietary fiber. Consider incorporating probiotic-rich foods like yogurt, kefir, or fermented vegetables to support gut microbiome health. A tablespoon of ground flaxseed daily can provide beneficial fiber and healthy oils that facilitate smoother bowel movements.
4. Type 4: Smooth, Soft Sausage (Ideal Stool)
Why this is considered optimal: Type 4 stools are the gold standard of healthy bowel movements. They’re smooth, soft, and snake-like or sausage-shaped with a consistency similar to that of toothpaste. They pass easily without straining and maintain their shape while being soft enough to exit comfortably.
What it indicates about digestion: Type 4 stools indicate optimal transit time through your digestive system—not too fast or too slow. This suggests your digestive system is functioning efficiently, with proper absorption of nutrients and water. It also indicates a well-balanced diet with adequate fiber and fluid intake.
How to maintain this type: Consume a balanced diet rich in both soluble fiber (found in oats, beans, and fruits) and insoluble fiber (found in whole grains and vegetables). Stay well-hydrated with water as your primary beverage. Maintain regular physical activity, manage stress levels, and respond promptly to the urge to defecate rather than delaying bathroom visits.
5. Type 5: Soft Blobs with Clear-Cut Edges (Lacking Fiber)
Appearance and characteristics: Soft, separate pieces with clear-cut edges that pass easily. These are often described as blob-like or resembling small, soft dumplings.
Causes and contributing factors: Type 5 stools typically indicate a lack of soluble fiber in the diet or slightly faster intestinal transit time than ideal. They’re common in people consuming low-residue diets or those who’ve recently increased their fluid intake without a corresponding increase in fiber.
Dietary adjustments: Gradually increase consumption of soluble fiber sources like oats, beans, apples, carrots, and psyllium husk. These help bind stool together for a more formed consistency. If you’re transitioning to a higher-fiber diet, do so gradually to avoid gas and bloating. Consider keeping a food diary to identify which foods contribute to improved stool consistency.
6. Type 6: Fluffy Pieces with Ragged Edges (Mild Diarrhea)
Appearance and characteristics: Fluffy pieces with irregular, ragged edges that are mushy and soft. These pass urgently and may be difficult to control due to their loose consistency.
Common causes: Type 6 stools often result from mild digestive upset, including mild food intolerances, mild infections, or irritable bowel syndrome (IBS). Stress, anxiety, and certain medications can also trigger this stool type by accelerating intestinal transit time.
When to be concerned: Occasional Type 6 stools aren’t usually concerning, especially if linked to an obvious cause like dietary changes or stress. However, if they persist for more than a few days, are accompanied by fever, severe abdominal pain, or contain mucus or blood, medical evaluation is necessary.
Management strategies: Stay hydrated with water, electrolyte solutions, or clear broths to replace lost fluids. Temporarily reduce high-fiber foods and focus on bland, easy-to-digest options like bananas, rice, applesauce, and toast (the BRAT diet). Probiotic supplements may help restore gut flora balance. Identify and address potential triggers such as certain foods, medications, or stress factors.
7. Type 7: Entirely Liquid (Severe Diarrhea)
Appearance and characteristics: Entirely liquid with no solid pieces, often resembling water. Type 7 stools lack any form and exit the body urgently and frequently, sometimes with little warning.
Potential causes: Infectious gastroenteritis (viral, bacterial, or parasitic) is a common cause. Food poisoning, certain medications (particularly antibiotics), inflammatory bowel disease flares, and intense emotional distress can trigger Type 7 stools. Toxins, excessive alcohol consumption, and malabsorption disorders may also be culprits.
Dehydration risks: This stool type poses a significant dehydration risk, especially in children, elderly people, and those with compromised immune systems. Watch for signs of dehydration including dry mouth, increased thirst, dizziness, reduced urination, and dark yellow urine.
When to seek medical attention: Seek immediate medical care if Type 7 diarrhea persists beyond 2 days in adults or 24 hours in children, or if it’s accompanied by high fever (over 102°F/39°C), severe abdominal or rectal pain, bloody or black stools, or signs of dehydration that don’t resolve with increased fluid intake.
Treatment approaches: Focus on fluid and electrolyte replacement through oral rehydration solutions. Avoid dairy products, caffeine, alcohol, and high-sugar beverages, which can worsen diarrhea. Over-the-counter medications like loperamide (Imodium) may provide temporary relief for adults but shouldn’t be used with certain bacterial infections or in young children without medical supervision. If an antibiotic is the cause, probiotic supplements may help restore gut flora balance.
Types of Poop Based on Color
8. Brown Stool (Normal)
Why stool is normally brown: The characteristic brown color of stool comes primarily from bilirubin, a breakdown product of red blood cells processed by the liver and released into bile. As bilirubin travels through your digestive system, it undergoes chemical changes due to bacterial action in your intestines, ultimately forming stercobilin and urobilin—compounds that give stool its typical brown hue.
Variations in normal brown color: Healthy stool can range from light medium brown to dark brown, with variations often reflecting dietary factors. Darker brown stools may result from consuming red meat, dark leafy greens, or foods rich in iron. Lighter brown stools might occur after eating a diet higher in refined foods or lower in meat protein. These variations within the brown spectrum are generally not cause for concern when other stool characteristics remain normal.
9. Green Stool
Causes: Green stool typically results from one of three primary factors: dietary influences, rapid intestinal transit, or medication effects. Foods rich in chlorophyll like leafy greens, green vegetables, matcha, or foods with green food coloring can produce a green tint. When food moves too quickly through the large intestine, bile doesn’t break down completely, resulting in a greenish hue. Certain medications, particularly iron supplements and antibiotics, may also cause green discoloration.
When it’s normal vs. concerning: Green stool following consumption of green foods or when taking certain supplements is completely normal and no cause for alarm. However, persistently green stools accompanied by diarrhea might indicate an infection or inflammatory condition. If green stools persist without an obvious dietary or medication cause, or if they’re accompanied by abdominal pain, fever, or other symptoms, consult a healthcare provider.
10. Yellow/Greasy Stool
Connection to fat malabsorption: Yellow, greasy stools that are bulky, foul-smelling, and may float or be difficult to flush often indicate fat malabsorption. When your body can’t properly absorb and digest fats, excess fat passes into the stool, creating a distinctive yellow or clay-like appearance with a greasy or oily quality.
Potential pancreatic issues: Chronic pancreatitis, pancreatic cancer, or cystic fibrosis can cause yellow, fatty stools due to insufficient pancreatic enzyme production. The pancreas produces enzymes crucial for fat digestion, and when this function is impaired, fat passes through undigested.
Other causes and implications: Celiac disease, which damages the intestinal villi needed for nutrient absorption, can cause yellow, fatty stools. Gallbladder removal or dysfunction affects bile release, which is necessary for fat digestion. Certain medications, particularly those that affect fat absorption like orlistat (a weight-loss drug), can also cause yellow, oily stools. Persistent yellow, greasy stools should always be evaluated by a healthcare provider, as they may indicate serious digestive disorders requiring treatment.
11. Black/Tarry Stool
Potential indication of upper GI bleeding: Black, tarry stools (medically termed melena) often indicate bleeding in the upper gastrointestinal tract—the esophagus, stomach, or first part of the small intestine (duodenum). As blood travels through the digestive system, it gets partially digested, resulting in a characteristic black, sticky, tar-like appearance with a distinctively foul odor. Common causes include peptic ulcers, gastritis, esophageal varices, or tears in the esophagus.
Medication-induced causes: Certain medications can produce black stools without bleeding being present. Iron supplements are the most common medication to cause harmless black discoloration. Bismuth subsalicylate (found in Pepto-Bismol and similar medications) combines with trace amounts of sulfur in the intestine to form bismuth sulfide, temporarily turning stools black. Some antacids containing aluminum hydroxide may also darken stool.
When to seek immediate medical attention: True melena (black, tarry stools resulting from bleeding) is always a medical emergency requiring immediate attention. If you experience black stools not explained by medication use, especially if accompanied by fatigue, weakness, dizziness, shortness of breath, or abdominal pain, seek medical care immediately. Blood loss from the upper GI tract can be substantial and life-threatening even before showing outward symptoms.
12. Red or Maroon Stool
Dietary causes vs. bleeding concerns: Red or maroon-colored stools can result from completely harmless dietary sources or potentially serious bleeding. Dietary causes include red food colorings, beets, cranberries, tomato juice or soup, and red gelatin desserts. These typically produce a more uniform red color throughout the stool. In contrast, blood in stool typically appears as streaks on the surface, maroon coloration mixed throughout, or bright red blood that’s separate from the stool.
Differentiating between harmless and serious causes: Dietary causes typically resolve within 1-2 bowel movements after the food is no longer consumed. Blood from hemorrhoids or anal fissures usually appears as bright red streaks on the outside of stool or on toilet paper. More concerning is maroon-colored stool, which may indicate bleeding from the lower intestinal tract. Bright red blood mixed with diarrhea could suggest inflammatory bowel disease, infection, or other significant conditions.
When to consult a doctor: Any unexplained rectal bleeding should be evaluated by a healthcare provider. Seek immediate medical attention if you experience significant amounts of blood, blood mixed with stool, persistent bleeding over several days, or if bleeding is accompanied by abdominal pain, fever, changes in bowel habits, or symptoms of anemia such as fatigue, weakness, or dizziness.
13. White or Clay-Colored Stool
Bile duct obstruction concerns: White, clay-colored, or pale gray stools (medically termed acholic stools) often indicate a lack of bile in the digestive system. Bile, which gives stool its characteristic brown color, may be absent due to blockages in the bile ducts from gallstones, tumors, strictures, or inflammation. Without bile, fat digestion is impaired, potentially resulting in stools that are not only pale but also unusually foul-smelling and difficult to flush.
Medication influences: Some medications can cause light-colored stools without indicating disease. These include certain antacids (particularly those containing aluminum hydroxide), barium sulfate (used in diagnostic imaging tests), and some anti-diarrheal medications. However, these usually cause temporary changes that resolve after the medication is discontinued.
Associated symptoms to watch for: Clay-colored stools are often accompanied by jaundice (yellowing of the skin and eyes), dark urine, itching, abdominal pain, and nausea when caused by bile duct obstruction or liver disease. These associated symptoms help distinguish potentially serious medical conditions from harmless, temporary causes. White or clay-colored stools that persist for more than a day or two, especially if accompanied by any of these additional symptoms, require prompt medical evaluation.
Other Stool Characteristics and Health Implications
14. Floating Stool
Gas vs. fat malabsorption: Floating stools can result from excess gas in the stool or increased fat content. Occasional floating stools due to gas are completely normal and often related to dietary factors that increase intestinal gas production. However, persistently floating stools, especially when accompanied by an oily appearance, strong odor, and visible oil droplets in the toilet water, may indicate fat malabsorption, where fats aren’t properly digested and absorbed.
Dietary influences: High-fiber foods like beans, whole grains, and certain vegetables can increase gas production in the intestines, causing stools to float temporarily. Carbonated beverages and foods high in lactose may have similar effects in sensitive individuals. These dietary causes of floating stool are generally harmless and resolve when diet changes.
When it might indicate a health issue: Consistently floating, foul-smelling, greasy stools suggest fat malabsorption, which may result from pancreatic insufficiency, celiac disease, or other digestive disorders affecting fat absorption. When floating stools persist for several weeks, particularly if accompanied by unexplained weight loss, diarrhea, or abdominal discomfort, medical evaluation is warranted to rule out malabsorption disorders.
15. Foul-Smelling Stool
Normal vs. abnormal odor changes: While stool naturally has an unpleasant odor, certain changes in smell can indicate digestive issues. Normal variations in stool odor occur based on diet and gut flora composition. However, extremely foul-smelling stools that represent a noticeable change from your normal pattern may signal health concerns, particularly when persistent or accompanied by other symptoms.
Dietary influences: Foods high in sulfur compounds, such as garlic, onions, broccoli, cabbage, and eggs, can cause particularly strong-smelling stools. Similarly, high-protein diets or the consumption of processed foods may intensify stool odor. These diet-related changes are typically temporary and resolve when diet adjusts.
Potential digestive disorders indicated: Persistently foul-smelling stools may indicate malabsorption disorders, where nutrients aren’t properly absorbed and instead ferment in the colon. Conditions like celiac disease, Crohn’s disease, or pancreatic insufficiency often present with particularly offensive stool odors. Intestinal infections, including those caused by Giardia, Clostridioides difficile, or other pathogens, typically produce distinctively foul-smelling stools, often accompanied by other symptoms like diarrhea. If unusually strong-smelling stools persist beyond dietary changes or are accompanied by other digestive symptoms, medical evaluation is recommended.
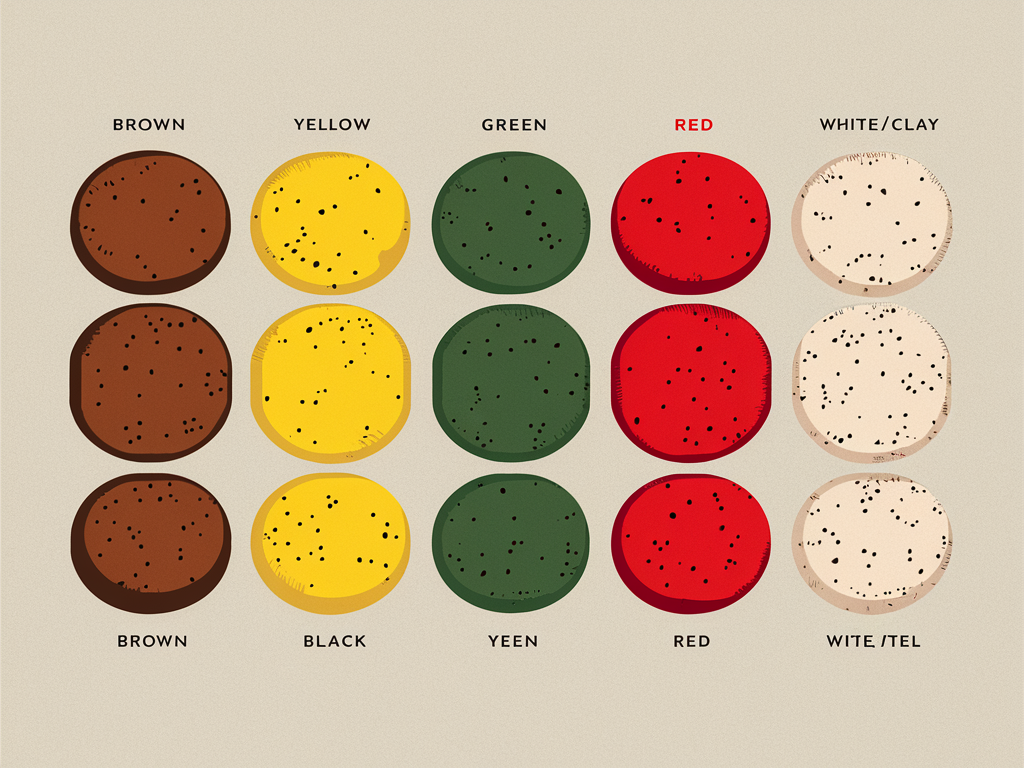
Comprehensive Stool Color Chart
Understanding the various colors your stool might present can help you identify potential health concerns. Here’s a reference guide to stool colors and their possible meanings:
- Brown (various shades): Normal, healthy stool
- Green: May indicate rapid intestinal transit, diet high in green vegetables, or iron supplements
- Yellow: Possible fat malabsorption, celiac disease, or giardiasis
- Clay/White/Gray: Potential bile duct obstruction, hepatitis, or certain medications
- Black/Tarry: Possible upper GI bleeding, iron supplements, or bismuth medications
- Bright Red: Potential lower GI bleeding, hemorrhoids, or certain foods (beets, red food coloring)
- Maroon: Possible bleeding in the lower small intestine or upper colon
- Orange: May indicate bile duct issues or consumption of certain foods/medications
- Blue/Purple: Typically caused by food dyes or certain medications

When to See a Doctor
Persistent changes in bowel habits: Any change in bowel habits that persists for more than two weeks warrants medical attention. This includes ongoing diarrhea, constipation, or alternating between the two. Changes in stool frequency, consistency, size, or shape that don’t resolve within a reasonable time frame should be evaluated, particularly in individuals over 50.
Warning signs that require immediate attention: Certain symptoms demand prompt medical care. These include:
- Black, tarry stools or bright red blood in stool not explained by diet or medications
- Severe, persistent abdominal pain
- Unexplained weight loss accompanying changes in bowel habits
- Chronic diarrhea, especially if accompanied by signs of dehydration
- Fever above 101°F (38.3°C) accompanying digestive symptoms
- Persistent vomiting alongside changes in stool
- Clay-colored stools, particularly if accompanied by jaundice
Screening recommendations: Even without concerning symptoms, regular colorectal cancer screening is recommended for average-risk adults beginning at age 45. Screening options include colonoscopy every 10 years or various stool-based tests at more frequent intervals. Those with a family history of colorectal cancer or polyps, or personal history of inflammatory bowel disease, may need earlier or more frequent screening. Always follow your healthcare provider’s recommendations regarding appropriate screening schedules based on your individual risk factors.
Factors That Affect Bowel Movements
Diet and hydration: What you eat and drink plays a fundamental role in your bowel function. Fiber content, particularly the balance between soluble and insoluble fiber, significantly affects stool consistency and transit time. Diets high in processed foods, animal proteins, and low in plant-based foods often contribute to constipation, while excessive sugar, spicy foods, or certain food intolerances can trigger diarrhea. Adequate hydration (typically 8-10 cups of fluid daily) is essential for proper stool formation and easy passage.
Medication effects: Many medications influence bowel function as either their primary purpose or a side effect. Common culprits include:
- Opioid pain relievers (often cause constipation)
- Iron supplements (may cause constipation and black stools)
- Antacids containing aluminum or calcium (frequently cause constipation)
- Antibiotics (can disrupt gut flora, leading to diarrhea)
- Magnesium-containing products (may cause diarrhea)
- Some blood pressure medications and antidepressants (can affect gut motility)
Always inform your healthcare provider about bowel changes when starting new medications.
Stress and lifestyle factors: The gut-brain connection is powerful, with stress and emotional states directly affecting digestive function. Chronic stress can accelerate or slow intestinal transit, potentially causing diarrhea or constipation respectively. Irregular eating schedules, shift work, travel across time zones, and poor sleep quality can all disrupt normal bowel rhythms. Creating consistent daily routines supports regular bowel function.
Exercise and physical activity: Regular physical activity stimulates natural contractions of intestinal muscles, promoting healthy transit time and preventing constipation. Even moderate exercise like walking can significantly improve bowel regularity. Conversely, sedentary lifestyles often contribute to sluggish bowel function. Incorporating movement throughout the day, rather than just scheduled exercise sessions, supports optimal digestive health.
Tips for Healthier Bowel Movements
Dietary recommendations: Aim for 25-30 grams of dietary fiber daily from diverse sources. Include both soluble fiber (oats, beans, apples) to add bulk and insoluble fiber (whole grains, vegetables) to speed transit time. Introduce high-fiber foods gradually to minimize gas and bloating. Limit processed foods, which can slow digestion and contain additives that may irritate the digestive tract. Include probiotic-rich foods like yogurt, kefir, sauerkraut, and kimchi to support a healthy gut microbiome.
Hydration guidelines: Water is the ideal beverage for digestive health. Aim for approximately 8-10 cups (64-80 ounces) daily, with needs varying based on activity level, climate, and individual factors. Increase intake when consuming high-fiber foods or during hot weather. Limit alcohol and caffeinated beverages, which can contribute to dehydration. If plain water is unappealing, try adding slices of citrus, cucumber, or berries for natural flavor without added sugars.
Physical activity suggestions: Incorporate at least 30 minutes of moderate exercise most days of the week. Walking after meals, particularly dinner, can stimulate digestion naturally. Simple exercises like gentle yoga poses (particularly twists), abdominal massage in a clockwise direction, and deep breathing exercises can help stimulate sluggish bowels. Even for those with limited mobility, chair-based exercises or gentle stretching can help maintain digestive function.
Proper toilet posture: Adopt a position that mimics squatting, which straightens the anorectal angle and facilitates complete evacuation. Use a footstool to raise your knees above hip level while sitting on the toilet. Lean slightly forward with elbows on knees. Relax and breathe normally rather than holding your breath or straining. Respond promptly to the urge to defecate rather than delaying, as postponement can lead to harder stools and constipation.
Conclusion
Your stool provides valuable insights into your digestive health and overall wellbeing. By understanding the various types based on consistency, shape, and color, you can better monitor your body’s signals and identify potential concerns before they become serious problems.
Remember that while occasional variations in bowel movements are normal, persistent changes warrant attention. The Bristol Stool Chart and the color guidelines provided in this article serve as helpful references, but they don’t replace professional medical advice.
Maintaining healthy bowel function is an important aspect of overall wellness. Through proper diet, adequate hydration, regular physical activity, and stress management, you can support optimal digestive health. Pay attention to your body’s patterns and don’t hesitate to consult healthcare professionals when concerning changes occur.
By being proactive about monitoring your digestive health, you’re taking an important step toward comprehensive wellness. After all, gut health influences not just digestion but immune function, mental health, and numerous other aspects of your overall wellbeing.

